Gleb Sukhorukov, Professor at Skoltech, Scientific Director of the LIFT Research Center, RSF grant recipient noted: “Speaking about coatings for therapeutic purposes, the scientific and medical communities face the problem of long-term retention of molecules. Our research group thought long and hard and eventually developed a microchamber technology where the substance is indeed retained for a long time. The advantage is that the drug is fixed inside the capsules in the polymer film, allowing for its sequential release into the wound. We expect to implement this technology into medical practice in less than three years. At the first stage, we managed to show that it does not cause harm. The next step is to prove a statistically significant therapeutic effect. I think within 1-2 years we will be able to confirm this.”
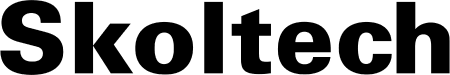
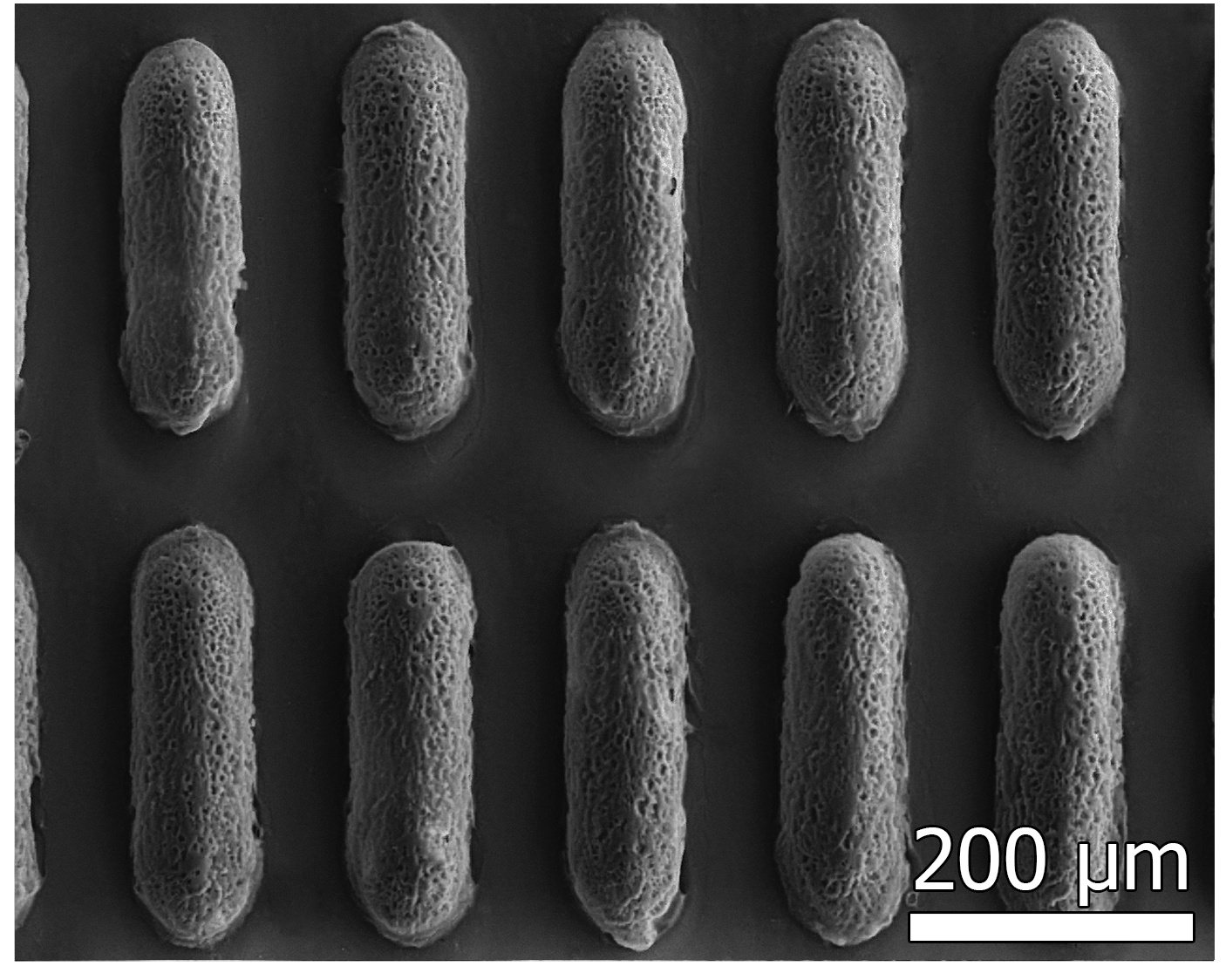
The researchers used a biodegradable polymer as a base, which should gradually break down in the wound, releasing the drugs. From this material, they formed highly ordered arrays of chambers, into which they “loaded” one of the bioactive substances — tannic acid or sodium percarbonate. The first compound is a natural antioxidant that reduces inflammation. The second serves as a source of hydrogen peroxide — an oxidizer that stimulates blood vessel growth and suppresses bacterial activity. The authors used these substances separately from each other (in different dressings) to precisely determine the effect of each.
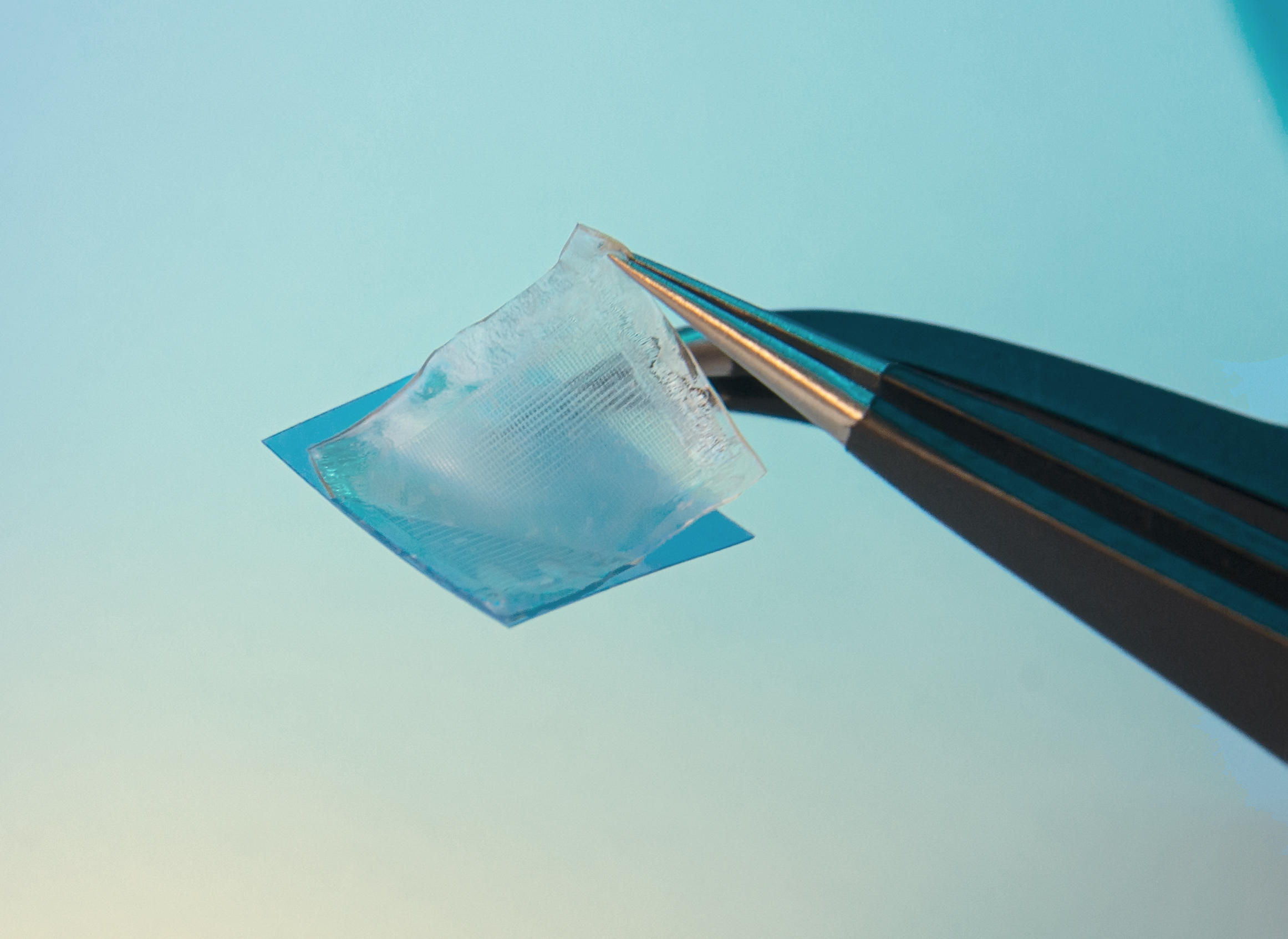
As a support material and the surface that should directly contact the wound, the researchers used a thin functional hydrogel film based on gelatin, glycerol, and aminocaproic acid. This combination of substances gave the material hemostatic properties, ensured its elasticity, moisture retention capacity, and reliable adhesion to living tissues.
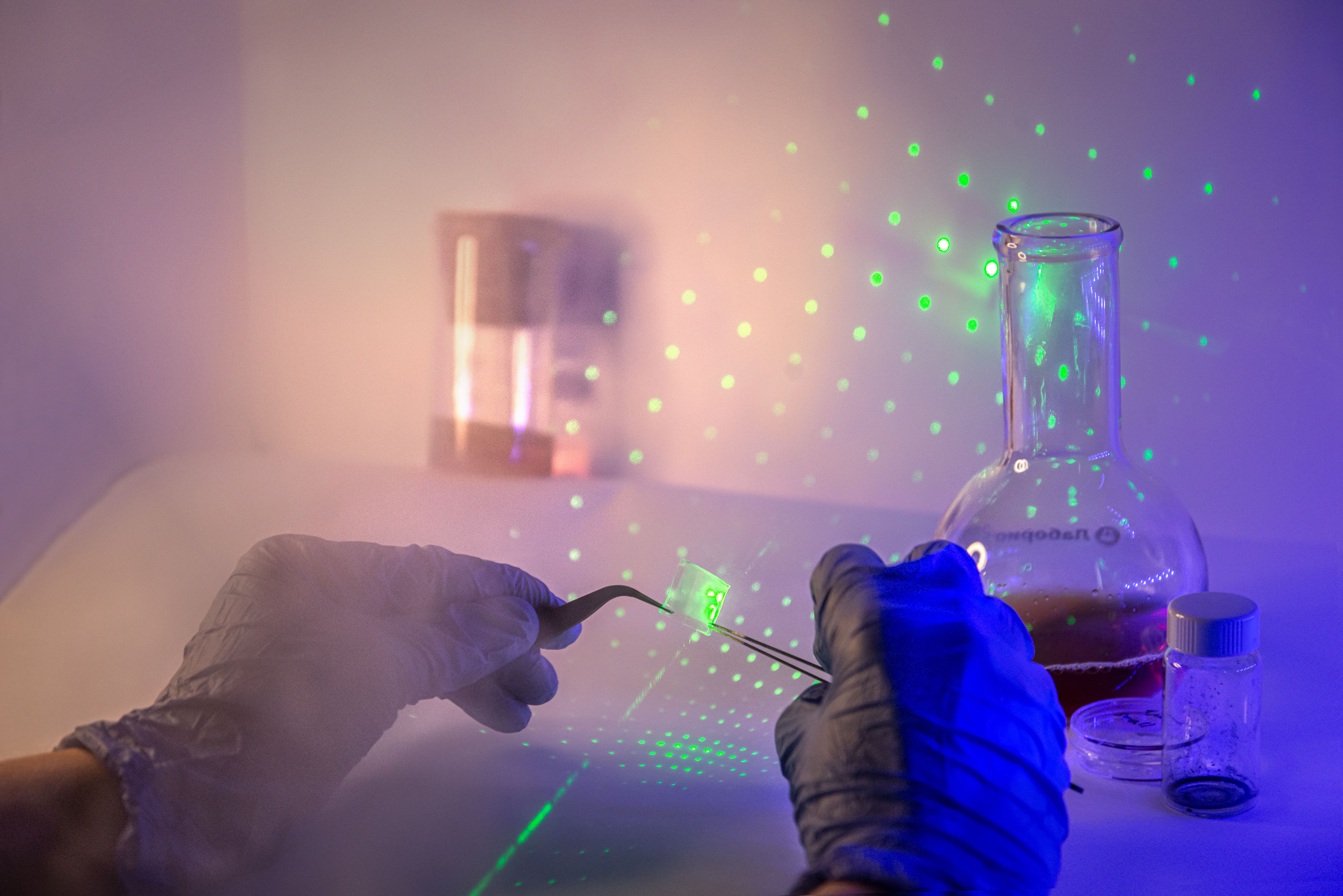
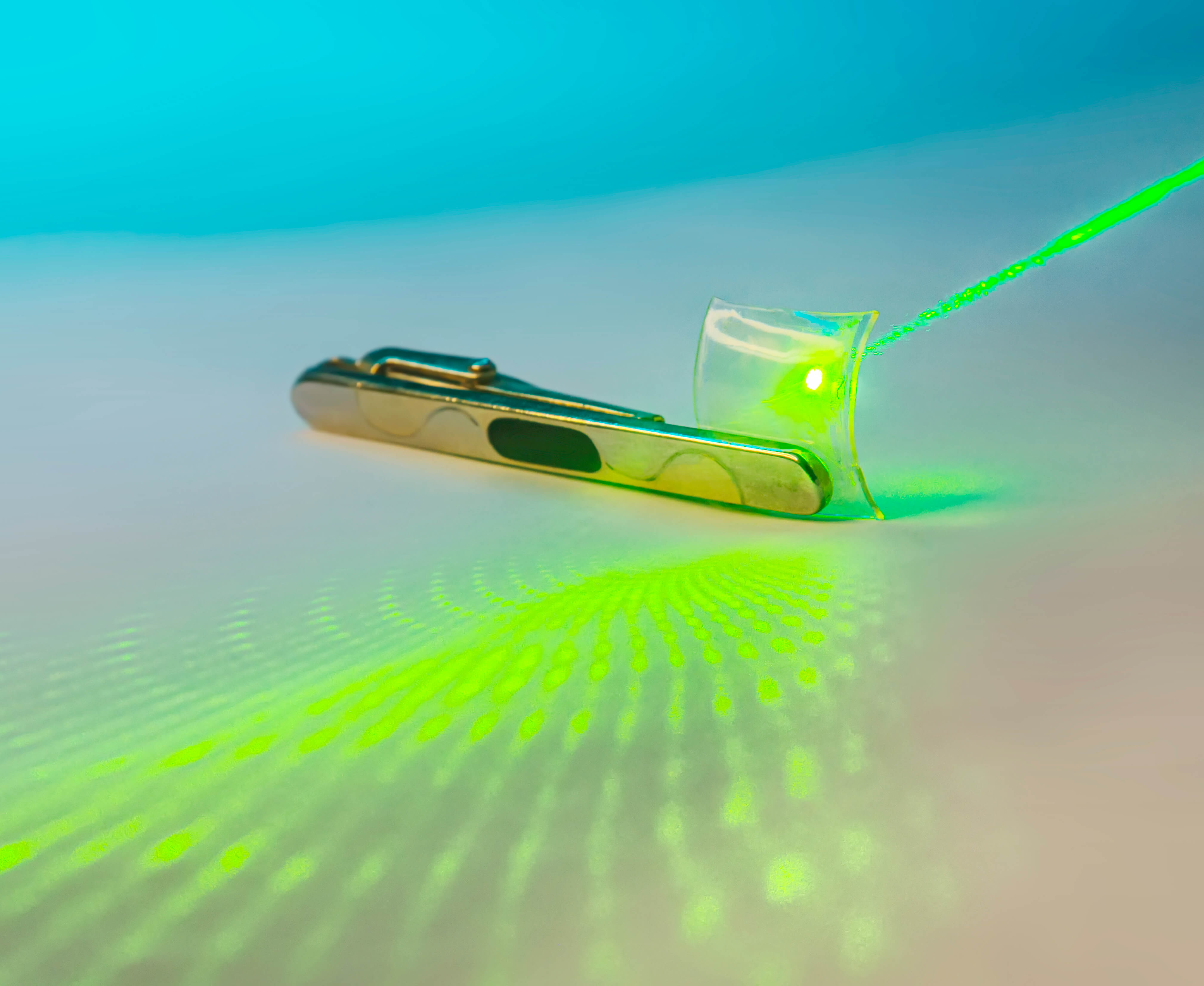
Laboratory tests confirmed that the developed system slowly releases bioactive substances from the chambers over 3-4 days. The authors emphasize that the speed of this process can be adjusted over a wide range by changing the composition or thickness of the polymer shell of the microchambers.
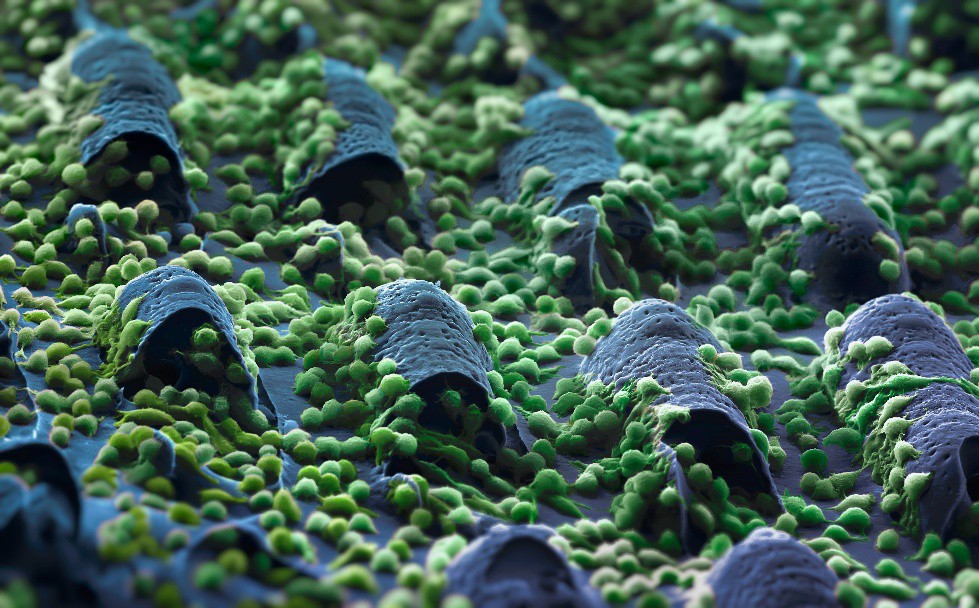
To test the material’s biocompatibility, scientists placed connective tissue cells — fibroblasts — on its surface. Under these conditions, the cells actively multiplied and maintained normal viability. Moreover, fibroblasts even penetrated into the cavity of the microchambers and formed a three-dimensional structure, indicating favorable conditions for healing.